Beyond The Skin
Diagnosis
- No clear consensus regarding the diagnostic work-up that should be performed when evaluating patients with AD, particularly adults, has emerged. Diagnostic approaches have large variation.1
- Chronic pruritus and itch induces scratch behavior, which can serve as a physiologic self-protective mechanism to prevent the body from being hurt by harmful external agents, but is well recognized to damage skin and increase inflammation, further exacerbating pruritus, resulting in the ‘‘itch-scratch cycle.’’2
- Clinical phenotypes and endotypes are characterized by a wide range of heterogeneity in the onset, course, and presentation of AD, as well as in individual comorbidities.
- The diagnosis of AD remains clinical, as there are no known reliable biomarkers that can distinguish AD from other diseases.3,4
- Guidelines of care for the management of AD issued in 2014 reported 28 different scales for the measurement of disease severity, without a single gold standard emerging.4
Figure 1: Patient-Related Challenges 11,12
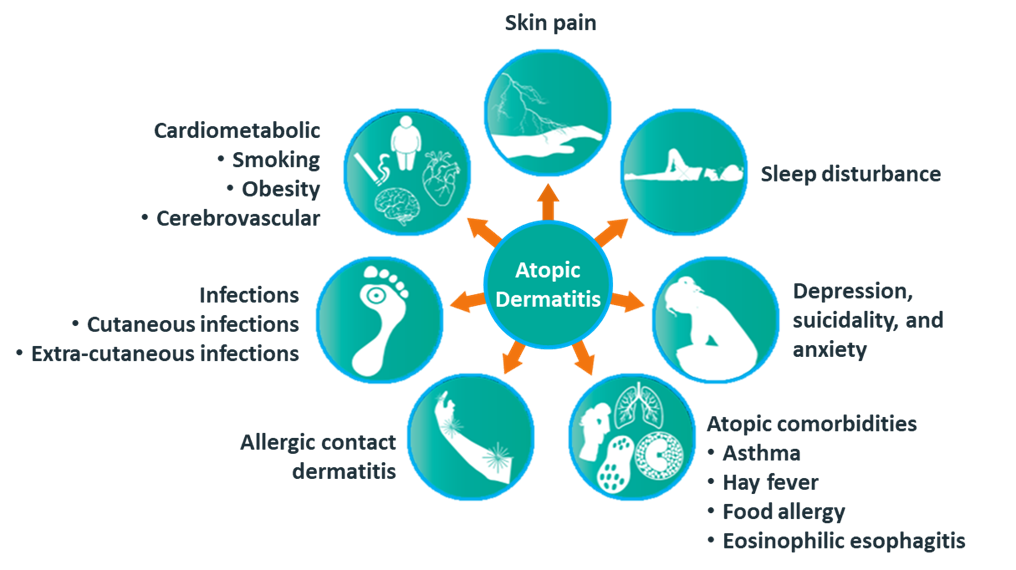
Patient-Related Challenges
- The propensity toward allergic disorders (asthma, food allergy, allergic rhinoconjunctivitis, and eosinophilic esophagitis) and skin infection (especially Staphylococcus aureus and widespread herpes/eczema herpeticum) is clearly increased in patients with AD.5-8 More severe AD appears to have a stronger association with asthma than mild or moderate AD.12
- Neuropsychiatric issues (attention-deficit/hyperactivity disorder, depression, anxiety, conduct disorder, autism, and suicidal ideation) have been recently linked to AD.5-8,12
- Assessment of disease severity is further complicated by a disconnect between physicians and their patients. The results of one study suggested that patients and physicians disagreed on the severity level of AD in approximately one-third of cases.9
- Maintaining motivation and treatment adherence in patients with AD is an important, yet often difficult undertaking.
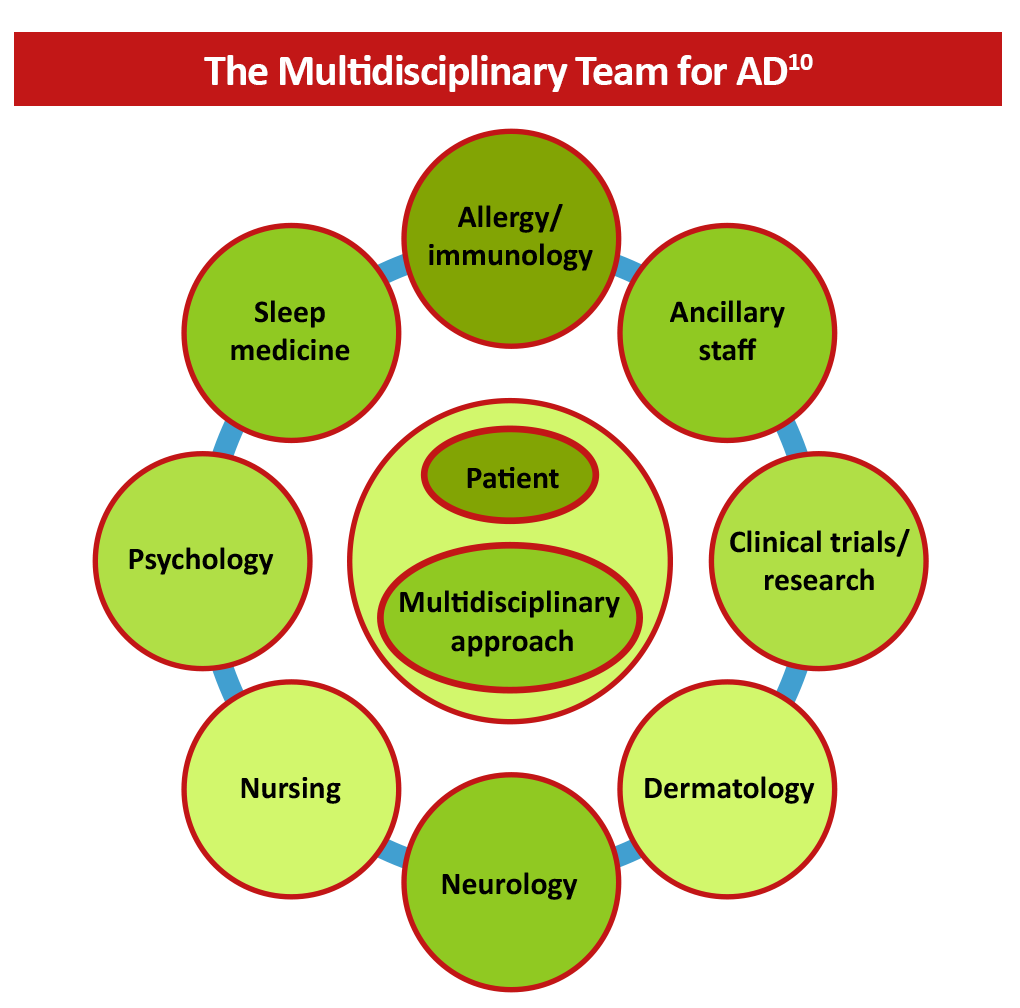
- Proper management of the direct and indirect effects of AD often requires expertise beyond the scope of dermatology. A multidisciplinary approach can treat common comorbidities, improve patient quality of life, reduce polypharmacy, and improve communication between providers.10
Figure 2: The Multidisciplinary Approach to AD 10
References
- Darsow U, Wollenberg A, Simon D, et al. ETFAD/EADV eczema task force 2009 position paper on diagnosis and treatment of atopic dermatitis. J Eur Acad Dermatol Venereol. 2010;24:317-328. https://doi.org/10.1111/j.1468-3083.2009.03415.x
- Paller AS, Kabashima K, Bieber T. Therapeutic pipeline for atopic dermatitis: End of the drought? J Allergy Clin Immunol. 2017;140:633-643. https://doi.org/10.1016/j.jaci.2017.07.006
- Silvestre Salvador JF, Romero-Pérez D, Encabo-Durán B. Atopic dermatitis in adults: A diagnostic challenge. J Investig Allergol Clin Immunol. 2017;27:78-88. https://doi.org/10.18176/jiaci.0138
- Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: Section 1. Diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol. 2014;70:338-351. https://doi.org/10.1016/j.jaad.2013.10.010
- Schmitt J, Romanos M, Schmitt NM, Meurer M, Kirch W. Atopic eczema and attention-deficit/hyperactivity disorder in a population-based sample of children and adolescents. JAMA. 2009;301:724-726. https://doi.org/10.1001/jama.2009.136
- Miyazaki C, Koyama M, Ota E, et al. Allergic diseases in children with attention deficit hyperactivity disorder: A systematic review and meta-analysis. BMC Psychiatry. 2017;17:120. https://doi.org/10.1186/s12888-017-1281-7
- Strom MA, Fishbein AB, Paller AS, Silverberg JI. Association between atopic dermatitis and attention deficit hyperactivity disorder in U.S. children and adults. Br J Dermatol. 2016;175:920-929. https://doi.org/10.1111/bjd.14697
- Thyssen JP, Hamann CR, Linneberg A, et al. Atopic dermatitis is associated with anxiety, depression, and suicidal ideation, but not with hospitalization or suicide. Allergy. 2018;73:214-220. https://doi.org/10.1111/all.13231
- Wei W, Anderson P, Gadkari A, et al. Discordance between physician- and patient-reported disease severity in adults with atopic dermatitis: A US cross-sectional survey. Am J Clin Dermatol. 2017;18:825-835. https://doi.org/10.1007/s40257-017-0284-y
- Nataloni R, ed. Multidisciplinary approach to eczema treatment. Dermatologist. 2016;24. https://www.hmpgloballearningnetwork.com/site/thederm/article/multidisciplinary-approach-eczema-treatment
- Silverberg JI. Comorbidities and the impact of atopic dermatitis. Ann Allergy Asthma Immunol. 2019;123:144-151. https://doi.org/10.1016/j.anai.2019.04.020
- Davis DMR, Drucker AM, Alikhan A, et al. American Academy of Dermatology Guidelines: Awareness of comorbidities associated with atopic dermatitis in adults. J Am Acad Dermatol. 2022;86:1335-1336.e18. https://doi.org/10.1016/j.jaad.2022.01.009