Diagnosis
Symptoms of prurigo nodularis (PN) include:
- itchy skin
- burning and stinging skin
- itchy bumps or nodules due to repeated scratching/picking that can vary in size, color, and number
- bleeding and painful skin as scratches break open resulting in dark spots and pebbly/hard skin
- scarring as the bumps clear1
Pruritis associated with PN is typically severe and episodic, but can be chronic, lasting longer than 6 weeks. Sweating, heat, clothing, and stress can aggravate pruritis.2 Among the most common causes of chronic pruritis, PN is thought to harbor the highest itch intensity.3
Diagnosis is based on clinical symptoms and responsiveness to treatment.
Other investigations include4, 5:
- A skin biopsy to help confirm a diagnosis; identifying characteristics include marked thickening and hyperplastic dermal nerve fibers with decreased intraepidermal nerve fiber density, increased number of neural mediators, and inflammation
- Direct immunofluorescence to rule out bullous pemphigoid, which can present as PN
- Patch testing to identify the presence of allergen triggers
- Blood testing to identify the presence of underlying systemic disease, which can include full blood count (FBC), liver, kidney, and thyroid function tests, and HIV tests
| Differential diagnosis6 |
|---|
|
Lichen simplex chronicus Hypertrophic lichen planus Pemphigoid nodularis Nodular scabies Keloids Dermatofibroma Foreign body reactions |
Pathology3
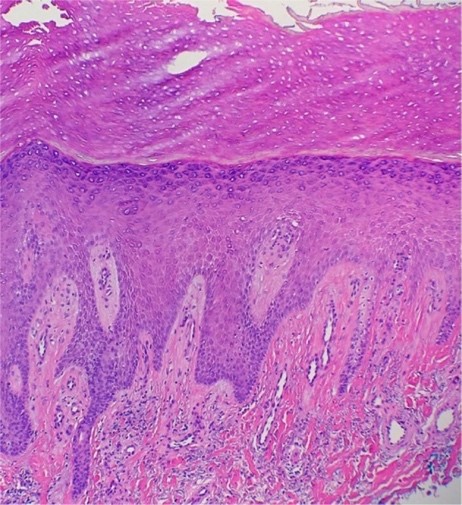
The most frequent epidermal features seen on a histological sample of a patient with PN include:
- Compact orthohyperkeratosis
- Irregular elongation of the rete ridges
- Focal or broad hypergranulosis
- Fibrosis of the papillar dermis with a vertical arrangement of collagen fibers
- Increased number of capillaries
- Inflammatory infiltrate composed mostly of lymphocytes and histiocytes
- White areas with peripheral striations, scaling, erosions, hyperkeratosis, crusts, and follicular plugging, red dots, and red globules3
Figure: Section showing orthohyperkeratosis, hypergranulosis, elongation of the rete ridges, vertical arrangement of collagen fibers, and increased number of capillaries3
References
- Ludmann P. Prurigo nodularis. American Academy of Dermatology Association (AAD). Updated 9/14/2021. https://www.aad.org/public/diseases/a-z/prurigo-nodularis-overview. Accessed 6/13/2023.
- National Organization for Rare Disorders (NORD). Prurigo nodularis. Updated 2/13/2023. https://rarediseases.org/rare-diseases/prurigo-nodularis/. Accessed 6/13/2023.
- Kowalski EH, et al. Treatment-resistant prurigo nodularis: challenges and solutions. Clin Cosmet Investig Dermatol. 2019;12:163-172.
- Gonçalves RB. Nodular prurigo. DermNet. Updated 7/2022. https://dermnetnz.org/topics/nodular-prurigo. Accessed 6/13/2023.
- Huang AH, et al. Prurigo nodularis: epidemiology and clinical features. J Am Acad Dermatol. 2020;83: 1559-1565.
- Mullins TB, et al. Prurigo nodularis. StatPearls. National Library of Medicine. Updated 9/12/2022. https://www.ncbi.nlm.nih.gov/books/NBK459204/. Accessed 6/13/2023.