Introduction
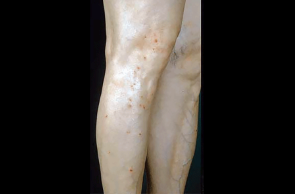
Prurigo nodularis (PN) is a chronic inflammatory skin condition characterized by the presence of pruritic nodules. 1 In the United States about 75,000 adults suffer from PN.2 Other names for this disorder include nodular prurigo, Picker’s nodules, atypical nodular form of neurodermatitis circumscripta, lichen corneus obtusus, and prurigo nodularis of Hyde.3 Lesions can vary in size from a few millimeters to 2 to 3 centimeters in diameter, ranging in number from a few to hundreds. Nodules may be flesh-colored, erythematous, or hyperpigmented and are typically located in symmetric linear arrangements along extensor surfaces of the extremities.1 Excessive scratching, picking, or rubbing of itchy skin leads to the formation of nodules, which typically develop on 1 or more of these areas: arms, legs, upper or lower back, buttocks, and abdomen.4 The persistent itching accompanying PN can lead to severe psychological distress and affect the patient’s quality of life.5 Patients report trouble sleeping, missing days from work, feeling sad/helpless, and having a limited social life.4
Figure: A-C: Examples of prurigo nodularis on legs (red, pink, skin-colored, or brownish black hard itchy bumps), arms, and hands; D: Example of itching leading to bleeding bumps4, 7



Epidemiology
While PN can occur at any age, it is often seen in middle-aged patients in their fifth or sixth decades of life and in individuals with darker skin color. Women are affected more often than men.1 Individuals of African American origin are 3.4 times more likely to be affected by PN than their White counterparts.6 The condition is commonly associated with other skin hypersensitivity disorders such as atopic dermatitis or chronic pruritis of diverse origin.6 It can also be associated with other underlying medical conditions such as cancer, diabetes, chronic kidney disease, or AIDS.3 Notably, PN may be predictive of advanced immunosuppression in HIV-positive patients.3
References
- Leis M, et al. Prurigo nodularis: review and emerging treatments. Skin Therapy Lett. 2021;26:5-8.
- Regeneron Pharmaceuticals 9/28/2022 news release. https://investor.regeneron.com/news-releases/news-release-details/dupixentr-dupilumab-approved-fda-first-and-only-treatment. Accessed 6/13/2023.
- National Organization for Rare Disorders (NORD). Prurigo nodularis. Updated 2/13/2023. https://rarediseases.org/rare-diseases/prurigo-nodularis/. Accessed 6/13/2023.
- Ludmann P. Prurigo nodularis. American Academy of Dermatology Association (AAD). Updated 9/14/2021. https://www.aad.org/public/diseases/a-z/prurigo-nodularis-overview. Accessed 6/13/2023.
- Satoh T, et al. 2020 guidelines for the diagnosis and treatment of prurigo. J Dermatol. 2021;48(9): e414-431.
- Mullins TB, et al. Prurigo nodularis. StatPearls. National Library of Medicine. Updated 9/12/2022. https://www.ncbi.nlm.nih.gov/books/NBK459204/. Accessed 6/13/2023.
- Gonçalves RB. Nodular prurigo. DermNet. Updated 7/2022. https://dermnetnz.org/topics/nodular-prurigo. Accessed 6/10/2023.